One of the questions I ask myself the most often when I am working with children and even with my own children, is, “is it sensory or is it behavior?” Working in schools, the sensory or behavior question is a big one. It comes up almost every time I am working with a kiddo. OTs and behaviorists are often in two schools of thought about this, but truly, the two go hand in hand. It is impossible to look at a behavior without looking at the underlying sensory components.
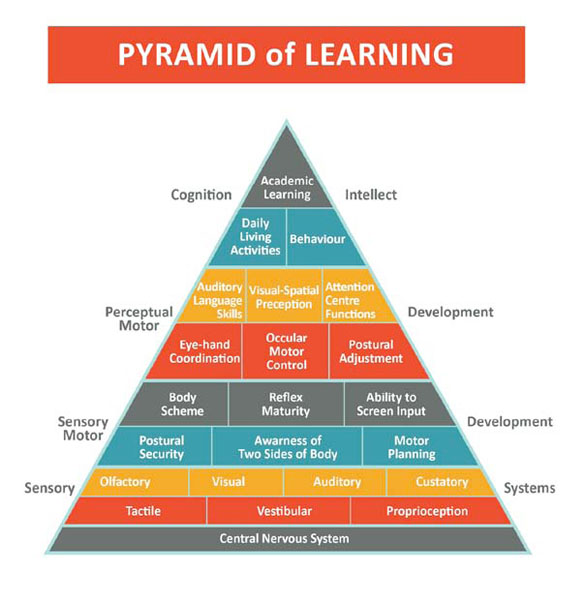
This pyramid is an excellent depiction of the role of sensory in behaviors…
Image retrieved from: https://www.otschoolhouse.com/episode26
The central nervous system is at the root of an individual’s functioning. From here, the tactile, vestibular (how we feel the effects of gravity) and proprioceptive (the push and pull of force on our muscles and ligaments so we know where our body is in space) are layered on. If there is a glitch here, in these 3 components, everything else that is stacked on top in the pyramid may be off. You can see behavior is near the top of the pyramid. Each of the components below, will affect one’s behavior. If a child cannot properly feel using their tactile discrimination or is overly sensitive to touch, you might see other senses heightened. They might seek more proprioceptive input. In the classroom, this would look like moving around in their chair, leaning on the desk, being too forceful with materials. If a child lacks vestibular integration you might see them touching everything, being too close to their neighbor when seated or in line. With these examples, a behaviorist might enter a classroom and see a child doing these things and institute a positive reinforcement system for sitting upright in class. Theoretically this is great. Positive reinforcement works. But the child will fail eventually because the sensory system has not been addressed. The child needs to learn strategies and teach their sensory system about what to do to help their body so that they CAN sit up and pay attention to the teacher.
As an OT and a Board Certified Behavior Analyst (BCBA), I approach the children with whom I work in a holistic way. I try to understand the family’s values first, how they structure their days, what the routines look like, get a pulse on how they operate and what habits make up their day to day. This is a critical part of what we do as OTs- understand the habits of people and with children, and that always involves the family. Understanding family dynamics, is extended family involved, are their older and younger siblings, what role does the family play in the behaviors? This can be difficult to obtain in the first meeting, but bits and pieces can be gathered and then continue to shape the occupational history about the kiddo and their family.
In the school setting, the same approach applies. It is critical to understand the teacher’s knowledge base, what sensory strategies they are familiar with, what classroom management strategies are in place, how the class operates, and what you can do to address both the sensory aspects and the resulting behavior. A big part of this is the environment as well. OTs are able to look at these various components that affect the child’s functioning. Assessing if the environment, both at home and at school, is too stimulating visually and auditorily. How are transitions throughout the day presented and executed? What antecedent strategies are in place to help the child from a sensory perspective AND a behavioral approach? This is where OT and behavior can really go hand-in-hand and OTs can provide sensory-based strategies to help get the nervous system “ready” for a transition, a particularly challenging activity, winding down and calming the body after said activity.
I have been at behavior conferences where inevitably, behaviorists scoff at the Wilbarger brushing protocol. This is an OT strategy that is often recommended to help children with tactile sensitivity and to provide deep proprioceptive input. Some OTs include it as part of a sensory diet at school or at home. While I agree that it would fall outside of the scope of what a behavior therapist is doing- understanding the underlying principles gives both an OT and a behaviorist the opportunity to collaborate, understand the child’s sensory needs, the resulting behavior, and what strategies CAN be put in place that can be executed by anyone working with the child.
I could go into many examples of when you might see a behavior and question if it is sensory-related or if it is a behavior. Instead, let these guiding questions help you discern what strategies need to be employed:
What time of day is it? - This could tell you if the child is tired, needs some down time, if it first thing in the morning and they had a full “good” night’s sleep you could begin to wonder if there is a sleep apnea related issue and consult your pediatrician.
Has the child eaten?- Did they have a balanced meal, did they just have a sugar-laden snack, was red-dye 40 in the food (there have been correlations between red food coloring and hyperactivity.
Was the child overstimulated?- This could be number of people, lights, they are in a big room or a very small room, is there a lot of background noise or loud noises.
Was the transition rushed or not explained prior to happening?- This is a big one and can even creep up at a time when you do not think that it would be an issue. Even if you think the child can be flexible or go with the flow, it is helpful to explain what is happening next or what behavior is expected of them prior to the transition.
Was something unexpected?- Was there an assembly at school that was not explained to the child, did the child need to leave a project or play that they were engrossed in, did something change from what they were otherwise expecting to happen?
Is something new?- New clothing that has not been shown to them prior to putting on could be difficult for some children to adjust to, the sensory aspects of the clothing might be noxious, the new straw cup you got them might feel different in their mouth, the new jacket has a zipper that is difficult to manipulate…
How is your energy as parent/ teacher/ therapist/ caregiver?- Children are so intuitive to the energy around them. Even at a young age, you might assume that they do not react to other’s emotions but they absolutely do. If you are frantic or anxious about something, chances are really good that the child or children around you feel it.
How is the behavior being reinforced? Is it getting a lot of your attention? Do you inadvertently strengthen it? Yesterday in 2nd grade I found myself calling on a kiddo who shouted out- it happened so automatically for both of us! Excited in the moment- neither of us could help it!
These questions above can help guide you in figuring out what is behind the behavior. Instead of then thinking about a punitive consequence to the behavior or a reward chart to shape the behavior, think about what you can do instead. Oftentimes, explaining what will happen next, what behavior is expected, what the child can do if they feel overstimulated, and teaching the appropriate replacement behavior can shape the behavior AND address the underlying sensory components. Praise goes a long way so then talking about what worked for the child (EVEN if the child is nonverbal!), what you noticed happened, what THEY noticed and how THEY felt will help strengthen that behavior so that it happens again in the future.
Tell me, what questions do you have? What examples come up when you think about this? It can be so hard to differentiate, so please comment and send me your questions!
Even 5 years late, she does not like dancing or performing!